A panel of representatives from the Asia-Pacific region will discuss how to scale up solutions to an alarming surge in HIV cases, during a WHO session this week.
New HIV diagnoses in Fiji have grown nine times more common over the last five years, according to the Fijian government, with many more cases likely undetected. The epidemic is driven by unsafe sex and by an increase in dangerous drug use as methamphetamine is trafficked through Fiji on the way to Australia and New Zealand.
The Science Media Centre asked experts to comment on the current situation in Fiji.
Dr Jalal Mohammed, Senior Lecturer, Faculty of Health, University of Canterbury and Adjunct Professor, University of Fiji, comments:
“The HIV/AIDS epidemic is ravaging Fiji. There is no other way to describe it. It impacts are not only being felt on the health of the population and its economic potential but also its social systems and structures. Reported new infections have surged by 3100 percent since 2010, and in 2025 alone, over 3000 new cases are expected to be reported. Unreported cases would significantly increase this number, with global estimates placing this figure up to 45% of this number.
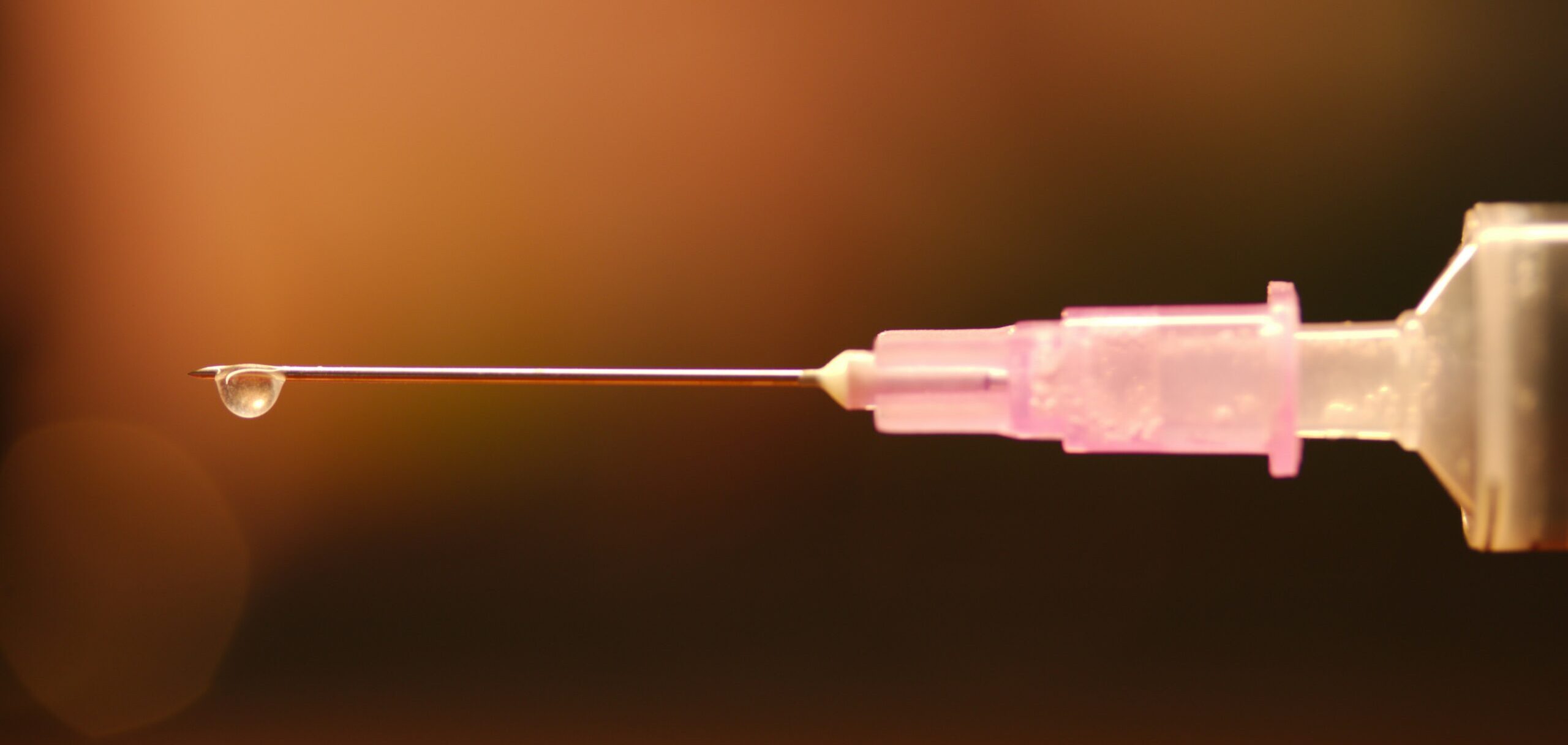
“Fiji’s already fragile health system is unequipped to deal with this epidemic. For decades the Fijian health service has struggled to deliver basic health services. Though investments are being made, it is not enough to halt the spread of the virus. This is because Fiji faces a larger problem. It is at the centre of the Pacific drug highway used by cartels to transfer drugs to larger markets such as Australia and New Zealand. As a side effect, drug trade and use have infiltrated all aspects of Fijian society. This has fueled the spread of HIV/AIDs with practices such as ‘chemsex’ and ‘bluetoothing’ – a practice where a drug user withdraws their blood after a hit to share with another person who can share the hit. This has fueled the rise in HIV/AIDS cases. We know from other countries where this practice has occurred, that new infection rates are amongst the highest in the world.
“I am in currently in Fiji, and you can see the health promoting messages to get tested being strategically placed on billboards and street light poles in Fiji’s capital, Suva – and much of the country. Currently new infections are being picked up through routine testing. To halt the spread, targeted health promotion messages around safe sex, regular testing, drug use, risks of needle sharing, advocated through social and community structures are needed. However, this is proving to be difficult due to the stigma that exists in a highly religious and conservative society. Combatting the stigma will be central to reducing the spread. Needle exchange centres are also needed. Pharmacies have clamped down on the sale of syringes, without prescriptions, under police pressure. However, a greater problem exists. ‘Bluetoothing’ has grown in popularity due to multiple people being able to chip in for a single hit to get high on.
“Hard drugs are also easily accessible, recently highlighted by international social media influencers touring Fiji. Central to reducing the spread of HIV/AIDS is reducing access and use of these drugs. This will be a challenge in a country with limited resources to establish drug and addiction services, and wrap around support services. A multisectoral approach is needed.
“Fiji is an important player in the Pacific and there is saying that what happens in Fiji is felt around the Pacific. As a major tourist destination visited by New Zealanders, we have a vested interest and as such we need to support Fiji and the Pacific in combatting the spread of HIV/AIDS.”
No conflicts of interest.
Dr Sharon McLennan, Senior Research Fellow at the School of Health, Victoria University of Wellington, comments:
“There are two key strategies which I believe offer some hope.
“First, an inward-looking strategy. Pacific culture and connections to the vanua (land, and cultural, social and spiritual identity) are strong. Traditional leaders remain highly respected and can play a powerful role in reducing stigma and leading local solutions.
“Secondly, external collaboration is vital. Australia and New Zealand, as key markets in the regional drug trade, share responsibility for addressing its impacts. Ongoing and coordinated support for regional anti-narcotics initiatives is crucial, as is addressing domestic drug demand. Health sector support and funding for infrastructure, prevention programmes and harm reduction must also be sustained.
“It is encouraging to see the WHO facilitating regional discussions on scaling up solutions. Real progress will depend on collective leadership, shared responsibility, and sustained commitment across the Pacific.”
No conflicts of interest.
Sir Collin Tukuitonga, Director of Te Poutoko Ora a Kiwa – Centre for Pacific and Global Health, comments:
“The surge in HIV cases in Fiji is a manifestation of poverty. The virus is being spread through intravenous drug use and the practice of blue-toothing, where a person injects drugs, withdraws blood and shares that blood with another person to share the drug’s effects. It’s a really confronting practice.
“Unfortunately, Fiji has been slow to set up needle exchanges. Politicians and leaders in Fiji are concerned needle exchanges would encourage drug use, even though evidence from around the world shows being able to inject safely doesn’t actually increase drug use.
“It’s been great to see the New Zealand Government contribute money to help control HIV in Fiji, as that helps fund testing and antivirals. However, there’s still a huge gap in global funding for HIV programmes since the US withdrew from UNAIDS and the World Health Organisation, so that will be impacting on Fiji.
“Part of the problem with HIV-AIDS is if you don’t test, you don’t know you’ve got it and that can speed the spread. So they are encouraging people to get tested.
“Although intravenous drug use is the biggest part of the problem, there’s an element of sexual transmission of HIV, particularly among gay men. In Fiji, attitudes to gay men and women can be unforgiving and discriminatory, so that might discourage people from identifying as gay or getting tested for HIV.
“Fiji is a popular destination for Kiwis, so it’s important the New Zealand public is aware about the risk of HIV in Fiji.”
No conflicts of interest.