Japanese scientists have grown functional human liver tissue – in mice.
The working human liver made using induced pluripotent stem cells was described in Nature this week. The liver is generated by transplanting liver buds (created in the laboratory) into mice, where the buds mature into tissue resembling the adult liver. Although it remains to be seen whether these techniques will work in human patients, the work provides a proof-of-concept that organ bud transplantation may represent a promising new approach towards regenerative medicine
Our colleagues at the AusSMC collected the following expert commentary. Feel free to use these quotes in your reporting. If you would like to contact a New Zealand expert, please contact the SMC (04 499 5476; smc@sciencemediacentre.co.nz).
Associate Professor Ernst Wolvetang, Group leader of the Stem Cell Engineering Group at the Australian Institute for Bioengineering and Nanotechnology and the University of Queensland, comments:
“Because of the shortage of donors for liver transplantation alternative strategies are needed. Reprogramming of the patient’s own skin cells into so-called induced pluripotent stem cells (iPSC) is an attractive option because it generates a type of stem cell that can generate every cell type of the body – their generation does not involve the use of embryos, and the resulting stem cells have the same genetic make-up as the patient’s own cells, thereby preventing rejection by the immune system.
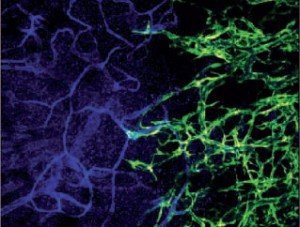
“The authors of this paper have used these cells to generate human liver cells and shown that when they are mixed with mesenchymal stem cells and blood vessel producing cells they can regrow a functional mature liver in mice. This provides proof of concept that this may be possible in humans in the future.
“It however remains to be established whether the artificially regrown livers from iPSC will prove to be safe in the long-term. The research clearly underscores the potential of induced pluripotent stem cell based regenerative medicine and highlights that similar approaches underway in Australian laboratories to regrow cells of the brain, kidney, blood, pancreas, lung, eye and heart from patient-derived induced pluripotent stem cells are worthwhile strategies for improving Australian health outcomes in the future.”
Professor Martin Pera, Program Head, Stem Cells Australia and Chair of Stem Cell Sciences at the University of Melbourne, comments:
“Human pluripotent stem cells can be multiplied indefinitely in the laboratory, and they can turn into any type of cell in the body. These properties mean that stem cells could be used in transplantation therapy to replace damaged organs. However, it has proven quite difficult to produce fully mature, functional human tissue from pluripotent stem cells grown in a petri dish. This exciting study shows that immature human liver cells, formed in laboratory cultures from pluripotent stem cells, can develop further and mature when they are grafted into a mouse.
“The grafted human livers have the full functional capability of the adult organ, such as the capacity to metabolise drugs. The results demonstrate that the rich and complex environment of tissues in the adult body can help immature stem cell grafts to develop to an adult stage. The report provides hope that even primitive tissues made from stem cells will one day restore function of dead or diseased organs in patients.”
Associate Professor Kiarash Khosrotehrani,Group Leader at the Experimental Dermatology Group at The University of Queensland, comments:
“Induced pluripotent stem cells (iPS) have raised the hope that in the near future, from a patient’s own cells, it will be possible to generate virtually any failing body organ. Liver failure is especially acute as it is a major vital organ and liver replacement by transplantation requires living or dead donors that are far too scarce.
“Despite their initial promises, turning iPS cells into liver cells has proved difficult. Numerous research groups, including major pharmaceutical companies, are trying to generate liver cells using iPS for transplantation, and also for pre-testing drugs to be released on the market. These attempts have in general been limited because of the difficulty in obtaining a mature (adult) liver cell population rather than an immature (fetal) liver that cannot do common tasks, such as producing albumin or metabolising drugs.
“This publication is a major step forward in the field as it presents evidence that maturation of iPS-derived liver cells can occur in experimental conditions, raising hope for future transplantation. The study also supports evidence from other groups regarding the major role of the blood vessels and stroma around these liver cells for their maturation and function. The latter is a feature being explored in many other areas of regenerative medicine, such as pancreatic islet generation for diabetes or vascularised bone graft generation for fractures.”
Associate Professor Kuldip Sidhu, Centre for Healthy Brain Ageing, University of New South Wales, comments:
“Growing mature tissues from both embryonic stem cells (hESC) and induced pluripotent stem cells (iPSC) is a state-of-the-art technology that scientists have been trialling for years. While some tissues like muscle and nerves derived from middle and outer layers of embryo are relatively easy to grow, others including liver, lung, thyroid and pancreas that all grow from the innermost layer of embryo, called endoderm, have been difficult to grow from stem cells in vitro. But, nevertheless, recently the significant convergence of frontiers of science like biomaterials, nano-biotechnology and tissue engineering, including molecular genetics, into the stem cell field has paved the way towards organ development.
“This paper is state-of-the-art, utilising not only these science frontiers, but also applying effectively the knowledge of fundamental developmental biology in organogenesis. It encompasses all the major components required in such an endeavour like the extracellular matrix, blood vessel forming cells and core liver forming endodermis cells (derived from iPSC in this study) to generate functional liver cells, albeit in mice. Similar studies in pigs will be useful as most of the organ sizes in pigs match with that of humans.
Growing human parts in animals may alleviate shortage of donor organs, but it does raise significant ethical and safety issues. Only a few countries, like Japan and the UK, have allowed the mixing of human and animal cells to produce chimeric embryos and to achieve organ production in animals. It does open up new vistas and hope for alleviating the suffering of those who need organ transplants.”