GLP-1 medications may be used to manage obesity, according to new guidelines released by the World Health Organization (WHO).
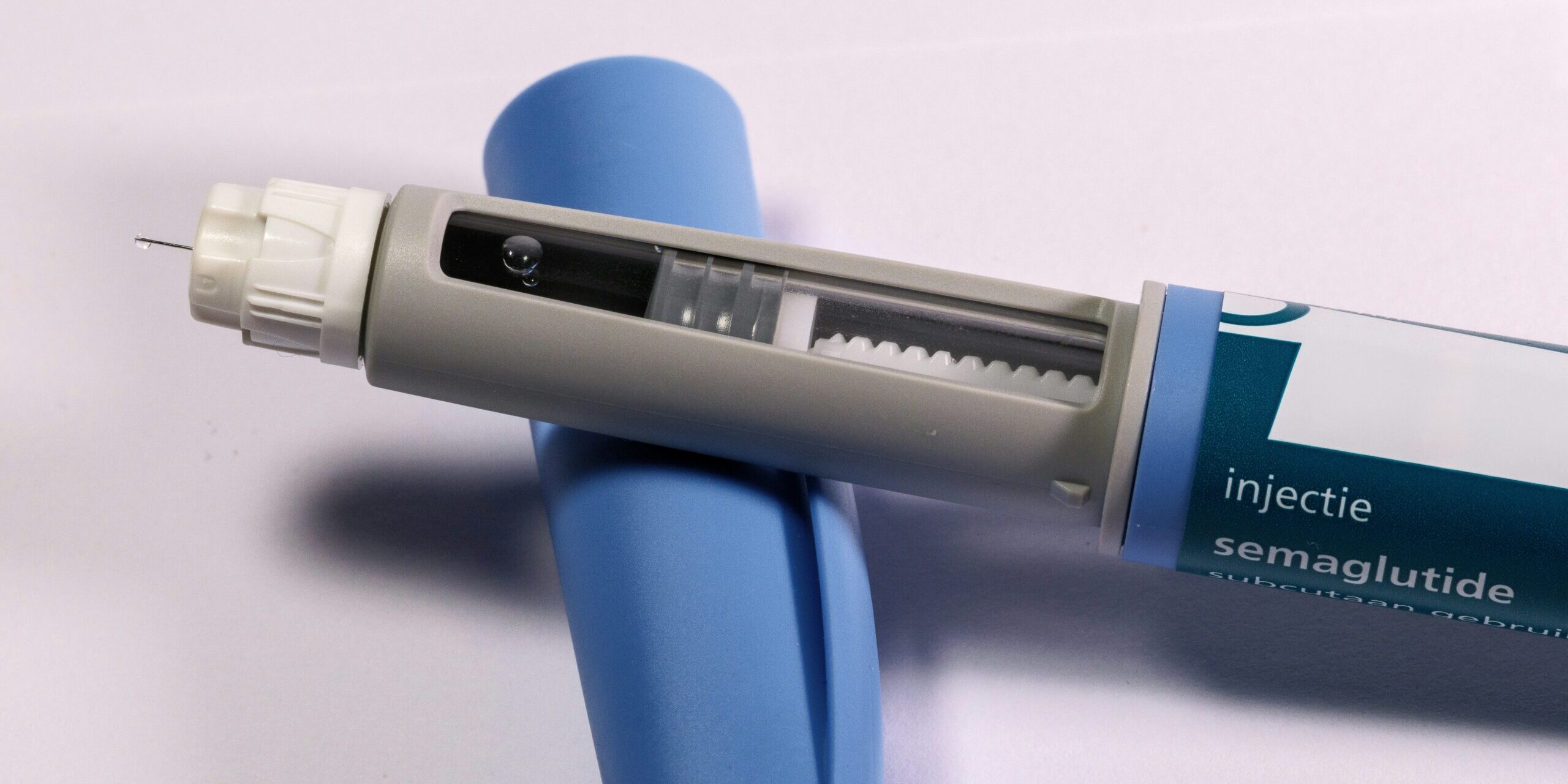
The WHO also recommends behavioural therapies, like changes to diet and exercise, along with the medications to sustain their benefits. The guideline’s recommendations are conditional for now, as more is still being learned about GLP-1 therapies like Ozempic and Wegovy.
The WHO emphasises that countries must ensure equitable access to affordable therapies, and that “medication alone cannot tackle the worldwide problem of obesity.”
The Science Media Centre asked experts to comment.
Professor Rinki Murphy, Department of Medicine, University of Auckland; endocrinologist and clinical head of Specialist Weight Management Service, Te Mana Ki Tua, Counties Health NZ Te What Ora; and diabetologist at Auckland Diabetes Centre, Te Toka Tumai, Health NZ Te Whatu Ora, comments:
“In New Zealand, obesity is still treated as a lifestyle issue, with no funded medications and only a limited number of publicly funded bariatric surgeries each year. Currently, prescriptions for GLP1RA are available only to those who can afford to pay for these medications which retail at around $500 per month, and very few prescribers offer integrated IBT, which is critical for sustained weight loss success.
“To ensure safe, cost-effective, and equitable implementation, New Zealand could start by restricting funding for GLP1RA based on clinical need, response to treatment, or limiting prescribing to clinicians with accredited obesity training or experience. Ideally, New Zealand needs to develop a nationally accredited obesity training program aligned with international standards, covering core competencies in pharmacotherapy, IBT, nutrition, and bariatric surgery, with a strong emphasis on cultural safety for Māori and Pacific communities. This program should include continuous medical education and have modules that extend beyond prescribers to be relevant for health coaches, support workers, dietitians, health improvement practitioners, and nurses to build a fully skilled multidisciplinary workforce who can help to combat obesity stigma and provide high quality, equitable, obesity care.”
Conflict of interest statement: “I declare my conflicts of interest as having advisory roles, speaking engagements and participation in steering groups for Lilly, Novo Nordisk, Boehringer Ingelheim, Abbott Diabetes Care.”
Professor Peter Shepherd, Molecular Medicine & Pathology, The University of Auckland, comments:
“This article highlights the next crucial steps required to ensure that the benefits of these drugs are maximised globally. One issue is cost. This is currently around $NZ6000 per year, and while many people report significant savings on food costs while on these drugs, this remains unaffordable for many individuals and also for Pharmac funding in this country. The good news is the patent for the main ingredient runs out soon and many competitors are poised to enter the market, so prices will surely fall.
“The other issue is what long term side effects might be. We already know muscle loss caused by these drugs is a potential issue, particularly in older people so careful monitoring will be required. However, the patient led demand driving the use of these drugs has led to the first ever reduction in rates of obesity in the USA, showing the people affected by obesity really want a solution. This article shows that global health bodies now recognise that medical treatments are now formally recognised as one important tool in reversing the tide of obesity.”
Conflict of interest statement: “I am involved in research projects to understand the molecular mechanisms driving the development of obesity and in projects to develop novel therapies for obesity.”
Associate Professor Lesley Gray, University of Otago, Wellington, comments:
“Even the word – obesity – draws wildly inaccurate societal views around an individual’s character or assumed behavioural flaws with many people still believing that obesity can be controlled by ‘eating less and moving more,’ – a very simplistic view of something that is in fact very complex with over 300 genetic, physiological, psychological, social, and environmental factors contributing to body size and body fatness, many of which are in fact beyond an individual’s control. The classification of a person’s height and weight as a disease are also highly problematic – we already know that weight based stigma and discrimination are in themselves harmful to large bodied people.
“GLP-1’s are a relatively new tool in the ‘weight toolbox’. Many tools have been tried and failed over the years, with weight and body fatness regain common. Even in weight reduction surgery, weight regain over time occurs for a large proportion of patients followed over a long time in research studies. We also know much more around harms associated with weight loss and weight regain. GLP-1’s are noted as a long term medication. but once these are stopped many bodies may start to regain weight. Weight is therefore not the best indicator of health improvement. A focus on cardiovascular improvements and other health markers provides more accurate measures of health improvement. Meanwhile, many of the contributing factors to increasing body size in populations remain relatively unchecked, e.g. access and affordability of high quality whole foods versus ultra-processed foods.
“GLP-1’s target the body mechanisms that regulate appetite and satiety, and they are not suitable for everyone. They do carry some significant possible side effects that need to be considered. For people who do believe they would benefit from these medications, there are currently major barriers in Aotearoa New Zealand given the monthly costs currently. This new paper concludes that such medications need to be universally available, accessible, affordable, and sustainable.
“I recommend a weight neutral, health-focused approach to health improvement and encourage, as a starting point, health professionals to learn about the potential harms of weight stigma and adopt trauma-informed approaches to care.”
Conflict of interest statement: “No conflicts relating to WHO or GLP-1’s. I do have a current Health Research Council project grant that is examining size inclusive aspects of the new HPV screening test as part of the cervical cancer programme.”
Professor Emeritus Elaine Rush, Auckland University of Technology, Riddet Institute, comments:
“The guideline identifies the challenge of ‘obesity’ and the need for more research on these drugs. Much is unknown – as stated, ‘What is needed is a comprehensive, system-wide response addressing prevention, care, and the underlying determinants of obesity.’ These drugs are expensive, and the recommendation is that intensive behavioural therapy and weekly counselling sessions are provided alongside the medication. Cost effectiveness is not known!
“We do know that for most obesity is a form of malnutrition, driven by the environment, i.e., a poor quality food supply, lack of physical activity, poverty, pollution, and it is intergenerational… a life course disease. Rather than invest in these drugs in the long term we should invest in reducing child poverty, (and improving school lunches) so that we support a better future and get a better return on investment in the long run.”
Conflict of interest statement: “No conflicts.”