Kiwi researchers have created maps of the country showing each region’s vulnerability to Covid-19.
They took into account Covid-19 risk factors like age, population density, and long-term health conditions – as well as ethnicity and awareness of health services.
The SMC asked experts to comment on the research.
Dr Jesse Wiki, GeoHealth Laboratory, Geospatial Research Institute, University of Canterbury, comments:
Note: Dr Wiki is a co-author on this research.
“Many factors can make populations vulnerable to adverse health outcomes and mortality related to COVID-19 including socioeconomic and demographic factors as well as pre-existing health conditions. Knowing who these population groups are, and where they are, can help inform the healthcare sector and support good health outcomes for the New Zealand population.
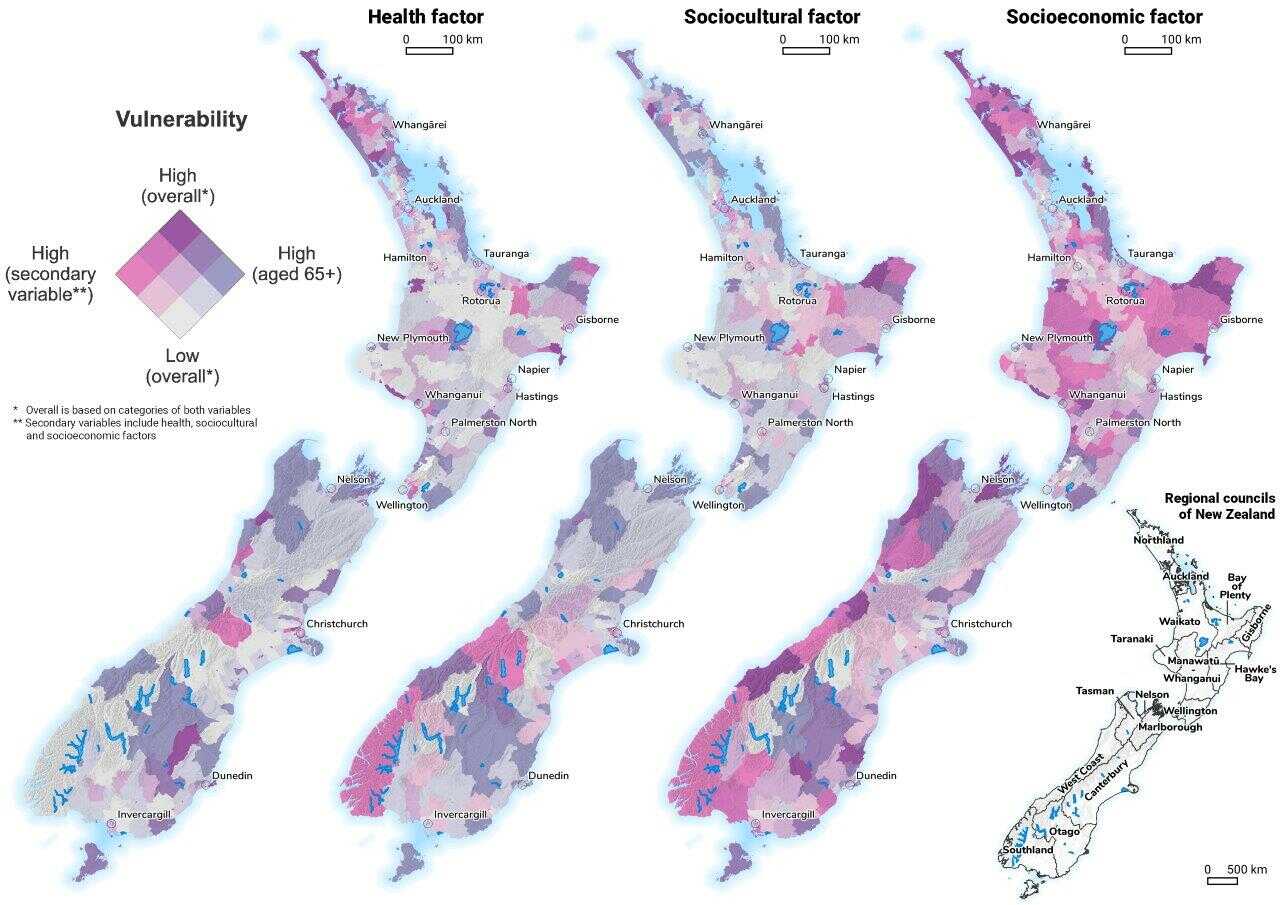
“Using data on a range of known risk factors and geospatial methods, we examined and mapped vulnerability nationwide. Results demonstrate unequal social and spatial vulnerabilities across New Zealand, with important distinctions based on health, sociocultural and socioeconomic factors. Interestingly, many areas of high vulnerability were located in small towns and communities, particularly those with large Māori populations. This is an important consideration given that such areas typically have less access to healthcare and fewer resources.
“By providing a spatial understanding of vulnerability this research can guide health‐focused policy to areas where interventions may be needed and generates information that can mitigate potential inequality in government response. It also provides support for the idea of targeted protective measures and precautions that can be effective locally, important considerations in the overall policy response.”
No conflict of interest.
Dr Amanda Kvalsvig, Epidemiologist, Department of Public Health, University of Otago Wellington, comments:
“This nice paper by Wiki et al. presents a very useful approach to pandemic planning.
“As the authors explain, vulnerability to Covid-19 depends on a number of factors including older age, disadvantage, background medical conditions, and smoking. These factors tend to occur together, creating a ‘syndemic’ situation where people experience multiple types of disadvantage, leading to multiple health issues. It’s complex: for example, one of the effects of colonisation is that Māori and Pacific populations overall have shorter life expectancy than other ethnicities. So there are a lot of people who are simply missing from the map, and others who are vulnerable at a relatively young age.
“While no analysis can capture all of the complexity, this type of approach is a huge advance on looking at health factors one by one. An important contribution of the paper is that the methods used to understand and communicate about overlapping risk factors could be used in many other ways: to plan the response to a new pandemic for example, or to map strengths and resources in communities across the country. Area-based information about strengths and risks has enormous value in a public health emergency because it can guide decision makers to get the right resources immediately to where they’re needed, without waiting for things to go wrong.”
No conflict of interest.
Associate Professor Collin Tukuitonga, Associate Dean Pacific, Faculty of Medical and Health Sciences, University of Auckland, comments:
“This study confirms findings from other New Zealand studies that some groups are at increased risk of COVID-19 infection, hospitalisation and death. Indigenous Māori and Pacific people are among the most vulnerable to viral infections, including COVID-19. Increased risk of COVID-19 infection and death is thought to be due to their adverse socioeconomic circumstances such as overcrowded housing and higher prevalence of co-morbid conditions, including diabetes.
“This study used geospatial methods based on the 2018 Census and existing databases, where they were able to demonstrate unequal social and spatial vulnerabilities across New Zealand. COVID-19 disproportionately affects older people and those with compromised health among other factors. Older age was the most significant factor affecting increased vulnerability to COVID-19. While these populations are at greater risk of adverse health outcomes and mortality from COVID-19, there are also known health inequities in care and access across New Zealand, particularly for ethnic minorities and those living in socioeconomically deprived areas. Areas with high Māori and Pacific populations are among the most vulnerable, including South Auckland and Porirua. Identifying where these areas of high vulnerability are located allows for better targeting of resources.”
No conflict of interest.
Dr Shanthi Ameratunga, Professor of Public Health and Epidemiology, School of Population Health, Faculty of Medical & Health Sciences, University of Auckland, comments:
“This study illustrates graphically why ensuring fair and equitable outcomes for the team of five million requires careful attention to the varying risks experienced by different communities. The maps show where there are greater concentrations of people at increased risk due to older age, underlying health risks (such as heart disease, diabetes, cancer, regular smoking), challenges receiving quality healthcare, and compounding factors of poverty and material hardship. With the notable exception of older age, most of these factors are disproportionately borne by Māori and Pacific peoples. This should spur focused attention to the unjust challenges borne by these communities.
“One aspect requiring more attention (and this is a common trap in many studies) is the dangers of averaging the experiences of highly diverse ethnic groups. The ‘Asian’ ethnic group includes both people with very high risks due to underlying health conditions (e.g., Indian communities with high rates of heart disease and diabetes) and those with low risks of these conditions. Combining them as one category could lead to misleading geographic concentrations of vulnerability based on ‘Asian’ populations as a group. The ‘MELAA’ category (only of use as a name that rolls easily off the tongue) has little meaning in a disease risk context as this covers people of Middle Eastern, Latin American, and African ethnicities. We have some way to go in acknowledging the multiple intersecting realities faced by these groups.”
No conflict of interest.