The Science Media Centre hosted an online media briefing with Dr Jemma Geoghegan and Dr Joep de Ligt about COVID-19 genomic sequencing and surveillance.
Dr Jemma Geoghegan is a senior lecturer at the University of Otago and Dr Joep de Ligt is lead bioinformatics with ESR.
Some of the briefing has been excerpted into a Q&A – the full briefing is available here.
Can you start by telling us about SARS-CoV-2, the virus that causes COVID-19 and what we have learnt about it so far?
Jemma Geoghegan
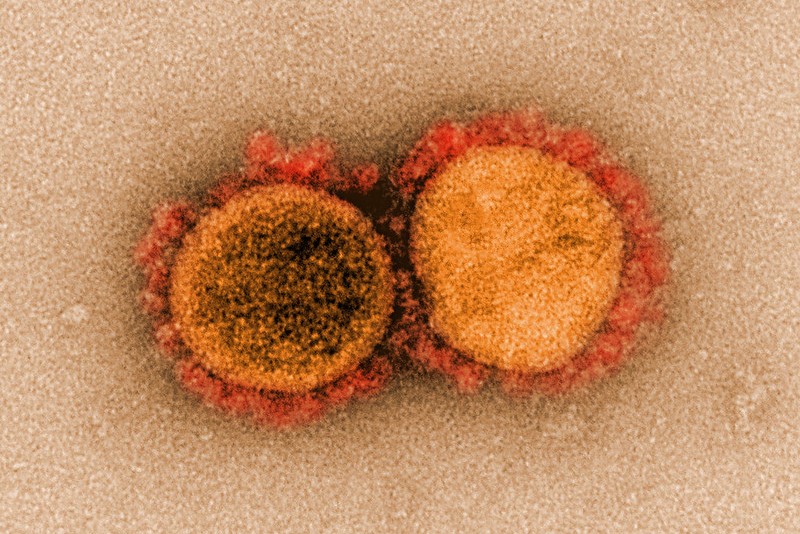
“This is a novel coronavirus which belongs to the family called Coronaviridae. These viruses in Coronaviridae have been known to infect humans before and some of these viruses cause diseases like the common cold. There have been two viruses that have caused more serious outbreaks, they’re SARS (Severe Acute Respiratory Syndrome) and MERS (Middle East Respiratory Syndrome) and they’re genetically related to this novel coronavirus.
“So in relative terms, our knowledge of the new coronavirus is actually quite remarkable. So if you think it was only five months ago that this virus was completely unknown to us and today it’s a subject of research on an unprecedented scale really.
“What we know about this virus so far, well we’re learning more every day. Like all viruses, it is evolving over time. How it evolves is it accumulates mutations and as the virus replicates inside a host it does that imperfectly, so these mistakes that the virus makes are mutations and they’re easily transmitted to the next person. However, saying that as a virus it is relatively stable because it does have some machinery that tries to correct some of those errors. This stability is actually a good thing because it doesn’t necessarily mutate as some other viruses do and that’s quite encouraging news for example in the hope of creating a long-lasting vaccine.”
Is there anything different that stands out to make this virus spread so easily?
Jemma Geoghegan
“I think the major difference is that Covid-19 infection is often a mild disease. That’s really the secret of the virus’ success. This means contagious people are unknowingly infecting others by walking around, transmitting the virus. So, by contrast, the disease that caused SARS, for example, makes people much more sick and it actually has a much higher mortality rate at around 10 per cent. When people are hospitalised, like they were often when they were infected with SARS, they weren’t going around infecting people which is the major difference here.”
ESR has been working to sequence the genome of the virus, can you briefly explain what this involves?
Joep de Ligt
“In the diagnostic laboratories they look for a small piece of the viral genome to determine if someone carries the virus or not, and that is when it becomes a positive case. Those cases that get a positive result are referred on to ESR to determine the complete genome structure of the virus. So it’s an RNA virus so we first translate it to DNA because most of the machinery that can read sequences they read DNA sequences and we also specifically amplify the virus which means that we make a whole lot of extra copies of the genome of the virus so that we study the virus and not actual hosts because we don’t want to see any human material. That is done on a sequencing machine.
“There are different models. The one we use for our rapid response is USB sized. There was an article talking about that earlier talking about how it can very rapidly determine the genome of the virus and if we then obtain the genome sequence we can look at those mistakes that might have happened (as Jemma was talking about). So the viruses that originate from Europe have slightly different mutations than the viruses that originate from, for example, North America and we can then use that information that is encoded in that genome to determine where the infection might have happened, but also more locally we can study if it is part of an outbreak that is already known so when you hear Dr Ashley Bloomfield talk about whether its an unknown source, or those kinds of investigations, they’re also assisted by that genetic information.”
How many tests can be done in a week, how long does it take to have results?
Joep de Ligt
“When we started out we did about 20 a week. We’ve since been ramping up capacity and implementing the new protocols as they’re coming out. As Jemma was saying this is a field of active research so protocols have been evolving and just today a new sequencer arrived at ESR that will double our capacity so we can now easily do 100 genomes a week and we are endeavouring to paint a complete picture as possible of the genetics of the virus in New Zealand and how it might have been spreading.
“In terms of the time for results, if it’s an urgent case we can have the result of the genome and the interpretation from that genome within a couple of days. The most important part is feeding that back to the public health units to try to determine if that is indeed in concordance with the genealogical data that has been collected in that case.”
What do we know about where this virus came from and how it got into humans?
Jemma Geoghegan
“The virus almost certainly originated in bats. There is a very closely related, similar virus called the RaTG13 virus which was sampled from a bat species in China. It’s possible that the virus first jumped on to an intermediate host before it jumped to humans. And that could possibly be a type of animal that had been in close contact with humans, perhaps at a live animal market for example.
“So we know that bats have likely transmitted the virus to other species of wildlife to because there is a closely related virus species that has been in pangolins, for example, that is a type of anteater.”
There have been rumours about the virus escaping from a lab, what does genomic data tell us about its origins?
“All evidence points to the fact that Covid-19 has naturally derived from a non-man-made source. And we know this by comparing the available data and genomic data from known coronavirus strains. It has been firmly determined the virus originated through natural processes.
“So the closest known relative of the virus is this bat virus. It’s being kept at the Wuhan Institute of Virology. So there has been a lot of unfounded speculation that the virus was the origin of the pandemic through a lab escape (or something similar) however this virus was sampled from a different province in China where Covid-19 first appeared and the level of genome sequence divergence between the virus that causes Covid-19 and this other bat virus – termed RaTG13 – is equivalent to about 50 years of evolutionary change so these viruses are very different.
“It’s very clear that it wasn’t an escape of this bat virus. Moreover. there have been no reports of people getting sick that worked in that virology institute lab and also finally the first outbreak of this virus was associated with a live animal market in Wuhan, which is exactly where we would expect this virus to jump hosts so all evidence points to this as a natural process.”
What role does genomic testing play in tracing the spread of the virus within New Zealand? Are there examples where this information has helped pinpoint where a case came from?
Joep de Ligt
“When new cases are being announced it often says they are under investigation, that means that people are still being interviewed and that people are trying to establish links to known clusters. Luckily in New Zealand we are doing a very good job of containing the virus so often due to that interview there’s already key links to known clusters or there’s good contact tracing because people are sticking to their bubbles. In some cases, it’s difficult to make that link either because it was some time ago the person had the symptoms and people can be asymptomatic for some time or just because the virus can spread so easily that you might not always make the connection. In some of those cases, we can then use the genome of the virus to identify a cluster that it is associated to. We may not always be able to ascertain that, but we can say it’s from a certain area or a certain event that we can link it to and therefore know how the transmission events might have happened.”
Do you have any specific examples of where a case origin wasn’t known and the genomic testing has helped point that back to where it came from?
Joep de Ligt
“One of the ones that has been followed up by the public health units was one where the genomics indicated that it was linked to the Queenstown outbreak and they followed up with that person and yes they were in the area but they didn’t necessarily have direct links to any of the events. But it is clear that somewhere during that time contact must have happened. So that’s one of the things we now know that it was unclear where that person may have been infected but we can now link it to that place.”
What does genomic surveillance data tell us about when and how the virus arrived in New Zealand and how has this changed since we closed our borders?
Joep de Ligt
“There’s very strong evidence that there have been multiple introductions into New Zealand based on the current sequence data and also work that has been done by the University of Otago. There’s an estimate that at the moment there’s at least 35 unique introductions. They’ve come from all over the world, so we’ve seen them from Europe, Iran, North America. Again this is consistent with what other countries have seen – that it is these international travellers that have brought it in in that narrow window before the borders were closed. After that border closure, we’ve not seen any new introductions or at least direct links to travel. This supports border closure as a very effective measure to prevent that further importation. It’s also now these local clusters that are making up these new infections.”
Initially we heard some discussion about there being more than one strain of the virus, particularly with regard to one strain being more dangerous – is there any evidence for this level of variation?
Jemma Geoghegan
“An early study suggested that there were two major types of this virus circulating the world. These two types were defined based on a few mutations in the virus’ genome. They concluded that there were differences in the rates of transmission between these two types. However, this conclusion was based on just a few mutations that differed between viral lineages and the conclusions were actually based on huge biases in the way the data had been collected because the numbers had major differences in different areas of the world, so that was the major problem with this.
“There’s actually hundreds of mutations that are present in the viruses genome already and that’s to be expected in any virus that’s continuing to circulate. But there’s no evidence to suggest that any of them will lead to changes in the way the virus behaves or transmits between people so I think it’s too early to say whether or not these mutations are causing any functional changes in the virus.”
What kind of changes in the virus will New Zealand – and the world – want to keep an eye on?
Jemma Geoghegan
“The virus is continually mutating, like any RNA virus does, so we need to monitor whether or not these mutations lead to any changes in the way that the virus affects us, or the type of disease it actually causes. So we need to know how much the virus changes because that will be really important in the future therapies like a potential vaccine or antiviral treatments and how effective they are in combating the disease.
All of this sharing of genomic data seems very open and rapid, how has that assisted with the global response to this pandemic?
Joep de Ligt
“It’s very impressive to see the world community coming together. The first genome sequence was very rapidly available and that allowed diagnostic lab groups to very rapidly develop diagnostic assays that can be scaled up to thousands of people a day. Also the understanding and the work that has been going on in terms of vaccines and potential antivirals or drugs – it’s happening at an unprecedented pace and I think that’s because with the genome of a pathogen people are quite willing to share that and to share learnings.
“Just two weeks ago I was part of a large international event called a hackathon, which means that they try to take all the data and look at what we can learn from that. It’s quite impressive to see the collaborative speed that is happening. We’re now at a point in time where we know much more about the virus than we knew and we’re just a couple of months in.”