 The results of the latest National Health Survey have been released, providing a snapshot of the health of New Zealand health and how has changed over time. Growing ethnic and and socio-economic inequalities, particularity in child and adult obesity rates, have raised concern.
The results of the latest National Health Survey have been released, providing a snapshot of the health of New Zealand health and how has changed over time. Growing ethnic and and socio-economic inequalities, particularity in child and adult obesity rates, have raised concern.
The survey contains information about smoking, nutrition, access to health care and oral health, based on data collected from 12,000 adults and 4000 children.
The new and improved National Health Survey, which started last year, aims to integrate a number of individual surveys that including the Adult and Child Nutrition Surveys, Tobacco, Alcohol and Drug Use Surveys, Te Rau Hinengaro (the New Zealand Mental Health Survey) and an Oral Health Survey.
The information collected is an important source of supporting evidence for health and health service policy and strategy development.
You can read more about the survey here. Several of the core findings for both the adult and child surveys are listed below.
Key findings from the adult survey include:
- Improving trends: reduced daily smoking, less psychological distress, fewer people unable to get an appointment within 24 hours, higher vegetable intake.
- No change: fruit intake, physically active.
- Worsening trends: obesity, diabetes, fewer dental visits.
Key Findings from the child (0-14) survey include:
- Improving trends: later age for introducing solid food, more general practitioner visits free for those under six years.
- No change: eating breakfast at home every day, asthma.
- Worsening trends: obesity.
One million obese Kiwis
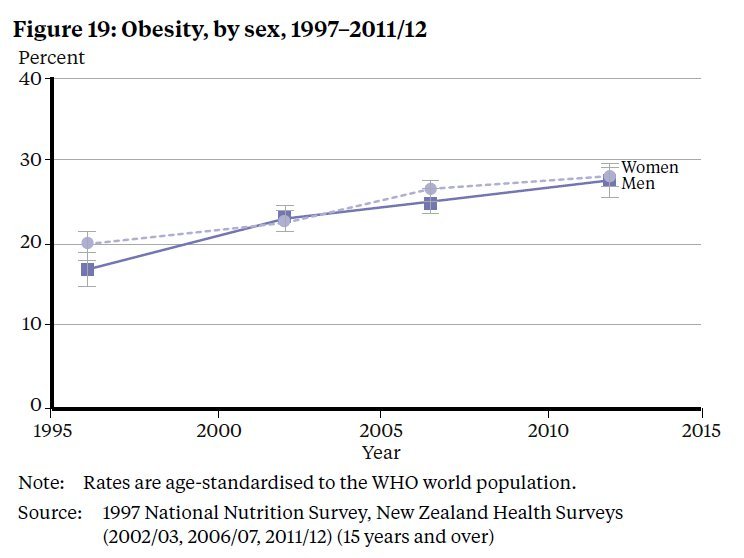 The survey data indicate there are about one million adults in New Zealand who are obese. Obesity rates have continued to increase over the past 15 years, from 19% in 1997 to 28% in 2011/12. The survey also found that there had been a substantial jump in obesity incidence among younger people; in the 15-24 year-old demographic the obesity rate has increased from 14% to 20% in the last 5 years.
The survey data indicate there are about one million adults in New Zealand who are obese. Obesity rates have continued to increase over the past 15 years, from 19% in 1997 to 28% in 2011/12. The survey also found that there had been a substantial jump in obesity incidence among younger people; in the 15-24 year-old demographic the obesity rate has increased from 14% to 20% in the last 5 years.
The children’s survey found that 10% of those aged 2-14 were obese, with rates higher among Maori (17%) and Pacific (23%) children, and children living in the most deprived areas (19%).
Obesity is a major risk factor for heart disease, type 2 diabetes and some types of cancer.
Inequalities highlighted
Both surveys also highlighted differences by population group with generally poorer health and more unmet need for health care among Maori, Pacific adults and children and people living in more socioeconomically deprived areas. Health inequalities in New Zealand came under public scrutiny in the year in the wake of research which showed dramatic rise in infectious disease rates over the last 20 years – with Maori, Pacific and poorer populations worst affected.
Condemnation from health expert
In response to the latest survey data Professor Tony Blakely from the University of Otago , Wellington, has called for action on child obesity. “I’m used to researching inequalities in health in New Zealand,” he said in a media release, “but I’m shocked by the latest figures on child obesity which show an increase rates from 8% in 2006/7 to 11% in 2011/12, and in particular the extreme inequalities that we now have in New Zealand. ”
“But perhaps the most shocking inequality is the six-fold gap between the most deprived (19% either obese or overweight) and least deprived (3%) neighbourhoods in New Zealand.”
“Some of this deprivation gap in child overweight/obesity is due to Maori and Pacific children being more likely to live in deprived areas, but the reality is that we now have extreme inequalities between rich and poor neighbourhoods. Not only does this create disparities in health now, but it bodes badly for diabetes, cardiovascular and cancer inequalities in the future if action is not taken.”
Actions to curb youth obesity suggested by Prof Blakely included:
- Banning all junk food advertising during children’s TV viewing hours
- Making sugar-free drinks the norm, not high sugar soft-drinks, through regulation, taxes and the industry stumping up to its responsibilities
- Ensuring schools and other public institutions provide healthy food
- Making healthy food the easy option for all New Zealanders, through subsidies or removing GST on fruit and vegetables combined with possible taxes on fatty and sugary foods (the impact of food subsidies and taxes was highlighted by New Zealand research just published this week).
If you would like to contact an expert for comment on any of the issues raised in the latest survey, please contact the Science Media Centre (smc@sciencemediacentre.co.nz; 04 499 5476)